What is Gastric Bypass Surgery?
Gastric Bypass is the weight loss procedure with the longest track record used in the treatment of obesity around the world. Gastric Bypass surgery is a combined restrictive/metabolic surgical procedure. It is restrictive in the sense that it ‘restricts’ how much food the stomach can hold and is ‘metabolic’ in that it influences gut hormones, blood sugar regulation, and metabolism.
This combination surgery has one of the highest success rates for amount of weight lost, making it a popular weight loss surgery option, especially for people with very high BMI’s (typically BMI >50) or type-2 diabetes.
The two most common types of Gastric Bypass surgery are the Roux-Y, and the One Anastomosis Mini gastric bypass. Other types of bypass include the SADI and duodenal switch procedures. Dr Taylor is experienced in performing all types of bypass surgery, and all are performed laparoscopically (keyhole surgery), using 5 small incisions. Dr Taylor will help you decide which option is best for you, but generally the One Anastomosis Mini gastric bypass is preferred for most patients as it has fewer side effects, unless you have severe gastro-oesophageal reflux disease, for example, significant oesophagitis or Barretts metaplasia, or smoke, or need to take regular anti-inflammatories for joint disease.
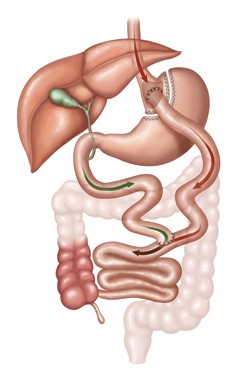
In Gastric Bypass surgery, a small stomach pouch is created by dividing the stomach into two using surgical staplers along the upper part of the stomach. The bottom of the pouch is then joined to the small intestine using sutures to allow food to exit the pouch (this is called an anastomosis).
This arrangement results in a small stomach and diverts food away from the top 1-2 metres of the small intestine, causing significant restriction as well as powerful metabolic effects that cause weight loss. These metabolic effects include beneficial alterations to gut hormones, improved composition of gut bacteria (the gut microbiota), and favourable changes to bile acid circulation. The Gastric Bypass is highly effective at treating diabetes, which improves in almost all patients, and put into complete remission, at least for a few years, in many. Most patients find they are able to keep their weight well controlled long-term.
However, the gastric bypass may also lead to a reduction in the absorption of certain micronutrients and vitamins, therefore ongoing supplementation and monitoring are important.
Advantages of Gastric Bypass Surgery include:
- The most amount of weight loss of the main procedures - most patients lose 60-80% of their excess weight, even if they are carrying a large amount of extra weight to start with.
- Excellent long term weight control - multiple studies show continued weight control at ten years and beyond
- Improved health problems associated with severe obesity, especially type-2 diabetes
- Improved mobility and quality of life
Am I eligible?
To be considered for the Gastric Bypass you will need to have a Body Mass Index (BMI) of at least 30. CHECK YOUR BMI
Health conditions including Type 2 diabetes, obstructive sleep apnoea, high blood pressure, joint osteoarthritis, slipped discs in the back, high cholesterol readings, and polycystic ovarian syndrome make the gastric bypass even more beneficial.
Talk to your doctor to find out more about your eligibility for a Gastric Bypass.
What are the risks of Gastric Bypass?
As with any surgery there are potential risks involved. Whilst most patients do not experience any problems after Gastric Bypass surgery, complications can occur with any surgical procedure and need to be considered when making an informed decision. Recovery and outcome may depend on the patient’s existing health status. Specific complications for Gastric Bypass surgery include:
- DVT (blood clot in the deep leg veins) and or PE (clot in the lungs)
- Leakage of digestive contents from staple lines or anastomoses which can lead to serious infections.
- bleeding
- Stricture (narrowing) of the opening between the stomach and small intestine
- Bowel twisting or obstruction caused by either kinking at the intestinal joins or internal hernias
- Dumping Syndrome: Vomiting, abdominal pain, and diarrhoea caused by stomach contents moving too rapidly through the small intestine
- Reduced absorption of key vitamins, minerals or protein leading to the risk of deficiencies especially if adequate supplements are not taken
- Gallstone formation
- Stomal ulcers (ulcers forming on the anastomosis) particularly in nicotine users (including vaping) or if NSAID anti-inflammatories are used regularly