The Sleeve Gastrectomy (also commonly referred to simply as “the Sleeve” has become the most commonly performed weight loss procedure worldwide, testimony to its effectiveness and excellent safety. Having performed more than 4000 gastric sleeves, it is also one of our favourite procedures at OClinic.
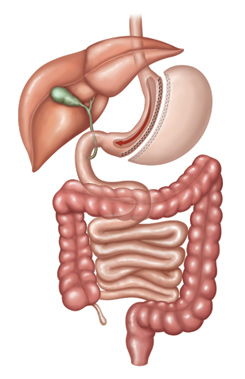
The Sleeve involves reducing the size of the stomach, which normally holds 5 cups, down to approximately 1-cup capacity. Using laparoscopic keyhole surgery under a general anaesthetic, the stomach is divided in two using surgical staplers, with the larger unwanted side removed. The removal of the unwanted side results in a 65% reduction in the amount of the hunger hormone Ghrelin.
People sometimes misunderstand the Sleeve as involving an implanted device- however this is incorrect- the Sleeve simply refers to the final shape of the new stomach- it becomes a small tube shape, like the sleeve of a coat.
The procedure takes one hour and involves 5 small incisions on the upper abdomen. Recovery is rapid, with patients able to walk about the ward with ease and consume a wide variety of fluids straight after surgery. The Sleeve only requires a one night stay in hospital, and 5-7 days off work.
It is very important that the sleeve is constructed properly, so the final shape of the gastric sleeve is even and consistent, without any twists or areas of narrowing. We frequently discover ‘hour-glass’ shaped sleeves with excessive stomach at the top and bottom but a narrow mid-section during corrective and revisional surgeries: This shape is associated with swallowing difficulties and reflux and must be avoided. The other concern is staple line leakage, which studies show is both less likely to occur, as well as better managed, if your sleeve procedure is performed by an experienced surgeon.
Although the physical size of the stomach is reduced, the normal direction of the food stream through the stomach and the rest of the intestinal tract is not altered. This means that all nutrients including vitamins, minerals and protein will continue to be absorbed in the small intestine normally. The stomach capacity is reduced from 1-1.5 litres to approximately 200mls, and this allows a person to feel comfortably satisfied and full with a meal size approximately equivalent to a cup of food, such as an entre.
Typically, Sleeve Gastrectomy patients will have between 3-5 small meals per day, which is actually the ideal way to eat. Dietitians recommend small frequent meals as a way of avoiding big swings in Insulin levels and achieving a more even intake of calories as part of a healthier eating pattern.
How does it work?
The Sleeve Gastrectomy appears to work in three distinct ways:
- Portion Control and restriction: The major reduction in stomach capacity allows patients to become full and satisfied with a much smaller meal.
- Hunger Reduction and taming of cravings: As the removed part of the stomach is rich in cells that make a hunger hormone called Ghrelin, the circulating blood levels of Ghrelin are reduced considerably after the Sleeve. Additionally, there is enhanced release of other gut hormones including GLP-1 and PYY after the sleeve that suppress appetite. As a result, patients report feeling less hungry, and have reduced sugar cravings after the sleeve gastrectomy.
- Improved Metabolism: A number of other beneficial changes have been shown to occur after the sleeve, including improvement in the bowel bacteria balance (the gut microbiome), gut hormones, and bile acid concentrations. These beneficial effects may explain why weight loss after bariatric surgery is more durable and longer lasting than from dieting alone.
Am I eligible?
The Sleeve Gastrectomy procedure may be suitable if you:
- have a BMI of at least 30 CHECK YOUR BMI
- have not been able to control your weight despite several genuine attempts at diet and exercise
- have stable mental health and no unmanaged addictions
- are at least 14 years of age
- are prepared to participate in long term medical follow-up
If you also have Type 2 diabetes, high blood pressure, sleep apnoea, polycystic ovarian syndrome, insulin resistance, fatty liver, or weight bearing joint issues, the sleeve may be especially beneficial in improving your health and longevity.
The Sleeve Gastrectomy procedure may not be possible if you have had some other types of surgery on your stomach organ in the past, such as removal of part of your stomach organ to treat cancer or an ulcer. But generally we are still able to perform the sleeve even after previous hiatus hernia or Fundoplication surgery, stomach stapling, endoscopic suture plication, or other types of weight loss surgery such as gastric banding. Please check with us if you have a history of any procedures on your stomach organ.
What are the risks of Gastric Sleeve?
Because the stomach itself has to be divided and then re-joined, one problem is that gastric fluid can leak through the staple line if there the healing along your staple line isn’t perfect. The risk of this complication in our experience is rare (approximately 1 in 300), and is suspected if a patient develops fevers and acute upper abdominal pain in the first week or two after surgery. Early treatment is the key to managing this problem successfully, so it is important to be on the watch for these symptoms and return back to the hospital without delay if concerns exist.
Other complications that can occur include internal bleeding, blood clots in the leg veins, intestines or lungs, infections in the chest or surgical wounds, and allergic reactions to anaesthesia or medication. These problems may occur following any surgical procedure, and precautions are taken in all patients to reduce these risks to the absolute minimum. Overall fewer than 1% of patients in our experience such problems, and these can be successfully treated with appropriate management.